Learning to Respond
I recently received the news that I was accepted to a Mindfulness Meditation Teacher Certification Program beginning February, 2021. I am excited to study with the incredible teachers Jack Kornfield and Tara Brach. Tara earned a PhD in clinical psychology and blends Western psychology with Eastern spiritual practices. Through her books, guided meditations and courses, she teaches millions of people around the globe to pay more attention to their inner life through mindfulness and compassion. I fell in love with her on the meditation app Insight Timer and one day received an invitation to apply to their program.
Jack Kornfield is equally impressive. Jack is credited for bringing Buddhist practices to the United States. After graduating from Dartmouth in 1967, he served in the Peace Corps in Burma. There he studied under Buddhist monks and was ordained as one in 1969. Upon his return to the United States, he co-founded the Insight Meditation Society in Massachusetts and the Spirit Rock Center in Woodacre, California.
My draw to the program is to deepen my meditation practice as well as to learn vocabulary and tools to teach. Mindfulness is at the core of both yoga and childbirth. I am certain it has enhanced my life and helped parenting. I know I want to be present for this journey. The years fly by and I don’t want to look back and feel like I missed it because I was in my head thinking about something in the past or planning for the future.
Parenting is tough. Whether it is calming a crying baby or referring a dispute between siblings, patience is paramount. And patience is a practice. I grew up in a household filled with love and kindness. But no one was afraid to yell. My hot temper did not fall far from my mama’s tree.
Shouting is a reaction - a reflex. It’s no different than being at my doctor’s office when she hits my knee with a tiny rubber hammer and it jerks straight. Responding is different. It is mindful. I can choose a response. But in order to do that, I need to be awake in the moment to understand that I am triggered and on the brink of yelling. I need space between the event and the response.
Viktor Frankl’s beautifully writes in Man’s Search for Meaning “Between stimulus and response there is a space. In that space is our power to choose our response. In our response lie our growth and our freedom.”
As a prerequisite for the Mindfulness Meditation Teacher Certification Program I am taking an online course called “The Power of Awareness”.. Tara Brach explained a technique as called STOP to create that space.
S: Stop what you are doing
T: Take a breath
O: Observe what is here
P: Proceed with presence.
The STOP idea is similar to something I learned in my yoga teacher training called “ABC.” In that technique, I created a 4 syllable mantra. Mine was “I.will.not.yell.” When something happened, the event, I’d take a mindful breath and ground my thumb on my leg and recite the mantra to myself, placing each of my other fingers on my leg in turn with each syllable. Only then would I choose my response.
A: A mindful breath
B: Beat
C: Choose my response
Both techniques are only useful when I remember to use them. However, it is a practice. I am grateful that I have the awareness of mindfulness. Knowing that life is finite, I want to be the best that I can be. I often think about the final lines of Mary Oliver’s poem “The Summer Day”
Tell me, what is it you plan to do
With your one wild and precious life?
Black Lives Matter
I was asked to be a guest blogger for Utah Doula Association. Here is my post:
The last few months have been filled with devastating news. 2020 in Utah will be remembered with the COVID-19 pandemic, earthquakes, and protests sparked by the murder of George Floyd by police officers. Our country and earth is in a place of unrest.
At the core of the unrest is systemic racism and racial inequality. Those of us who work in the birth world are acutely aware of the disparities for Black mothers and babies. In the New York Times Magazine article, “Why America’s Black Mothers and Babies are in a Life and Death Crisis” author Linda Villarosa states that “Black women are three to four times as likely to die from pregnancy-related causes as their white counterparts, according to the C.D.C.” and “black infants in America are now more than twice as likely to die as white infants — 11.3 per 1,000 black babies, compared with 4.9 per 1,000 white babies, according to the most recent government data.”
The racial inequalities during COVID are even worse. The latest data show that African Americans have died from the disease at almost three times the rate of white people. New figures compiled by Color of Coronavirus provide further evidence that across the country, African Americans have died at a rate of 50.3 per 100,000 people, compared with 20.7 for whites, 22.9 for Latinos and 22.7 for Asian Americans.
Understandably, people of color are angry. The members of UDA are angry. People across the globe are angry. Black lives matter.
Families and businesses have been affected. The Utah Doula Association (UDA) is no exception. Following in the footsteps of many other individuals and businesses, the weekend of June 5th, the UDA posted a message of solidarity on their social media. The UDA acknowledged the indignities and dangers our Black sisters and brothers have lived with for generations, and committed to rebuild injustices and be ally champions.”
The June 5th statement was rejected by a member of our community. She felt it was insincere, and that the UDA has a lot of work to do to remedy years of members feeling undervalued or unheard.
She, and some other members of our community who identify as doulas of color asked the UDA board for a meeting. On June 10th, the doulas and the board connected over Zoom. The doulas of color shared their perspectives, including the painful truth that they did not always feel safe, heard, or valued through the UDA. The board of the UDA listened intently.
The work of uncovering and addressing the UDA unconscious bias has now begun. Without this conversation, the white doulas on the board or in the UDA at large did not fully understand what it was like for the doulas of color. Even though the conversation was difficult for all who participated, it was a key to learning and growing.
As the best-selling, anti-racist writer, Ibram X. Kendi recently said in an interview with Brené Brown (listen here): “The heartbeat of anti-racism is confession, is admission, is acknowledgment, is the willingness to be vulnerable, is the willingness to identify the times in which we were being racist; is to be willing to diagnosis ourselves, and our country, and our ideas and our policies. And the reason why that’s the heartbeat is, like with anything else, the first step is acknowledging the problem. You know, we can’t even begin the process of changing ourselves, of acting in an anti-racist fashion if we’re not even willing to admit the times in which we’re being racist.”
Love, kindness, and compassion are an innate aspect of being a doula. It was extremely difficult to hear that some doulas of color have felt marginalized by UDA on that June 10th Zoom call. However, we know they spoke their truth. Everyone committed to listen and learn.
There is meaning and importance in diversity, equity, and inclusivity. The members of the UDA board have realized that they have a blind spot. Improvement will be made to strengthen the organization, but it will take work.
The UDA is committed to do the work.
A week later, the board met again and agreed on the following, which was posted on social media:
The UDA has been made aware that some members of our organization and our birthing community do not feel safe or heard by the Utah Doula Association. We value ALL doulas and seek to uplift the voices of ALL underrepresented individuals especially Black, Indigenous, People of Color, and those who identify as LGBTQIA+. As a group of compassionate advocates for birthing and postpartum individuals and families, we commit to an intentional effort to remove barriers and create spaces of inclusivity. We recognize that this work is ongoing. Over the next 12 months, the UDA will:
1. Provide anti-racism education to individuals and the organization to understand both
interpersonal and systemic racism, provide specific doula training to navigate racism in
the labor room, and provide tools for full-spectrum doula work;
2. Develop an Access and Inclusion committee, which we hope will include diverse and
professional voices in equity and equality;
3. Reevaluate UDA processes and bylaws to promote equity;
4. Foster more community and collaboration within the organization through social and
professional gatherings.
Through these actions, the UDA hopes to create a space of inclusion and trust for those who have previously felt unseen within our doula community. If you have feedback for the UDA, please take a moment and fill out this form. Your identity will remain anonymous, if you choose. We appreciate you and value your opinion; thank you for speaking up.
Though the road ahead is uncertain, there is no doubt that through the rise of the Black Lives Matter movement, diversity, equity, and inclusion will be on the forefront of every decision made in the future. We are grateful to all the doulas in the Utah doula community for their perspective.
In the words of Maya Angelou, “Do the best you can until you know better. Then when you know better, do better.” The UDA is on the road to better.
An OMazing Year
Happy Birthday OMazingBirth! My business turned one this past month. I am proud of my work and progress as a doula and educator:
I attended thirteen births in the past twelve months. After each birth, I drop a rock into a jar in my studio. Every birth I attended was filled with opportunity to grow and learn as a doula. The support that I provided undoubtedly was appreciated by the couple. But I often left feeling like the lucky one. I saw a new life born. It does not get old. Pam England wrote, “Birth is magical, not mystical” which I have come to understand in a deeper meaning. There are both similarities and differences in every labor and birth. The more of them I witness, the more I understand. A year later, I feel more comfortable in a birth room.• Yoga in my OMazing Studio flourished. I created a small community of new and expecting moms who practiced together or often just with me. The vibe is exactly as I imagined: warm, calm, and peaceful. Every student I taught appreciated the flexibility of the intimate setting. If their sleeping baby woke up, I paused the class. No big deal. Maybe the baby went back to sleep or maybe she joined her mama on the mat. Or some days, I held a baby while her mama practiced pigeon or rested in shavasana. The OMazing studio provided space to breathe, practice and relax. • Teaching at the University of Utah in their Perinatal Education department has been an honor and a challenge. The hospital is incredibly progressive. I appreciate the opportunity to teach diverse couples preparing for childbirth. Teaching my first couple of classes was hard! Being comfortable in the uncomfortable is a practice. However, the energy of the room is worth the work. Every student I encounter is excited to become a parent. Their hope fills me up. Simultaneously, I’ve learned so much being on the faculty. The University is dedicated to professional development. Last week I attended a staff meeting to discuss the ARRIVE study. (A Randomized Trial of Induction Versus Expectant Management) The researchers carried out the study to find out if elective induction of labor (using medicine to start labor without a medical reason) during the 39th week of pregnancy would result in a lower rate of death and serious complications for babies, compared to waiting until at least 40 weeks and 5 days for elective induction. They also wanted to see if inductions had an effect on the risk of Caesarean sections. (To read the results of the study, click here.) It has been widely debated and controversial. One of the lead doctors on the project is a University of Utah doctor. He participated in our staff meeting sharing the results of the study and his perspective. He answered our questions and was genuinely curious about our opinion. It was like being at the Sundance Film Festival in a Q&A with the film director. I loved it.• Six months ago, I created Hive Family Collective with two local women who are now my partners and friends. Hive focuses on connecting and educating postpartum families. We filed the paperwork in April to obtain 501(c)(3) tax exempt status. Every Tuesday morning, we host a weekly coffee for new moms called NewBee Mamas. Candace Roper, a local lactation specialist joins us every week to provide support and answer questions. When new moms connect, I am reminded of the importance of this work. Anyone who has a baby knows the fear and uncertainty of the first year. Everything is new. The lack of frame of reference is disorienting. Instead of wondering “is this “normal” in isolation, Hive Family Collective provides conversation to help build confidence, community and connection. In addition to to NewBee Mamas, every first Tuesday of the month, Hive Family Collective hosts a speaker to provide education and perspective. A local pediatrician, mental health counselor, behavioral sleep specialist and mind coach all donated their time and expertise to Hive this year. We are looking forward to the work ahead especially as we tip toe out of quarantine. • I hosted a workshop called “Rites of Passage” with a soul-sister, Heather DeFord this spring. We met with a handful of middle-school girls three Friday afternoons and talked about their changing body. Heather is a pelvic floor physical therapist and is passionate about anatomy and ritual. We shared facts about the female body and mensuration and educated the girls. In a safe space, we encouraged them to ask questions. We talked about what it means to be a good friend and how to navigate life at school. The girls gained both some new knowledge and few new friends. They created a text group and called it “love (heart emoji) my body” . That’s what we want, right? Middle school girls who love their bodies.• Lastly, over the past year I have deepened my meditation practice. I witness the mind body connection not just in labor but also in parenting. Personally, I am on a journey to become a more present, calm parent. When I create space between an event and my reaction the outcome is better (read: calmer). I breathe and give myself a chance to choose a response. It’s a work in progress but I am seeing progress. As a teacher, I focus on mindfulness in my childbirth and yoga classes. Pregnancy is a fantastic entree into this world of mindfulness. The mom’s are sober, clear and able to connect with their baby. Realizing that I want to formalize my training, I recently applied to Tara Brach and Jack Kornfield’s two-year Mindful Meditation Teacher Certification Program and was accepted. I look forward to learning and sharing my insights. The world needs more meditation. I really appreciate your support in my inaugural year of OMazing. It is truly a pleasure to work in this space. I am grateful to have you join me in my journey!
Racial Disparity in the HealthCare System
Mid-April I participated in a national webinar hosted by the Doulas of North America during Black Maternal Health Week. Their focus is health equity. Jennie Joseph, a respected health advocate for women and newborn babies led the webinar and she was fired up. She told the doulas on the call to move from awareness to action; to join her in the perinatal revolution. The time is now. I felt a little uncomfortable sitting in my beautiful OMazing studio listening.
A couple of years ago I read a chilling New York Times Magazine article, Why America’s Black Mothers and Babies are in a Life and Death Crisis by Linda Villarosa. That day, I learned that, according to the CDC, black women are three to four times as likely to die from pregnancy-related causes as white women - a rate higher than Mexico, where nearly half the population lives in poverty. I remember being stunned to learn that American Black infants are more than twice as likely to die as white infants: 11.3 per 1,000 black babies, vs 4.9 per 1,000 white babies. Ms. Villarosa points out that this racial disparity is worse than in it was in 1850, 15 years before the end of slavery. Shamefully, the US is one of thirteen countries in the world where the mortality rate is worse today than it was twenty-five years ago.
These statistics are abhorrent.
Racial disparities are not isolated to the health care system. They are deeply rooted inequalities across society, politics and the economy. There are many reasons why black women have worse birth outcomes than white women. The stress of living with racial bias can contribute to complications in pregnancy like hypertension and pre-eclampsia. Those conditions can lead higher rates of infant and maternal loss. Vallarosa writes “societal racism is further expressed in a pervasive, longstanding racial bias in health care — including the dismissal of legitimate concerns and symptoms — that can help explain poor birth outcomes even in the case of black women with the most advantages.”
This is not a class issue. This crisis exists for black women across all socio-economic populations.
My good friend, Nyitur is South Sudanese. She and her husband have suffered terrible racism in this country. To such an extreme they are in the middle of a malpractice lawsuit. Andrew suffered a stroke in 2014 and was misdiagnosed. First the doctors treated him like a drug addict. Next, they thought he had malaria. He had no use of his left side. Hours passed before he was diagnosed and treated for a stroke. Six years later, Andrew is still unable to talk in complete sentences and will never work again.
Eight months after Andrew’s stroke, Nyitur gave birth to her daughter Athiei. She arrived at the hospital in active labor. She knew birth was imminent based on her three previous births. Her contractions were strong and painful. Her three older children were born rapidly so she was anxious to settle into her hospital room. When she arrived at the hospital, the Labor and Delivery nurse performed her routine cervical check. She proclaimed Nyitur was not dilated enough to be admitted. They sent her home. Both adamantly and politely Nyitur begged to stay. She knew the baby was coming soon. The nurse firmly refused. “You don’t know. Every birth is different”. Defeated, Nyitur and her friend Susan left the hospital and drove twenty minutes home to Nyitur’s apartment. Less than ten minutes later they were on their way back to the hospital. Fortunately, the nurses admitted her because in less than an hour later, Athiei was born.
I wonder, if based on my whiteness if I would have been able to convince the nurse to let me stay? I don’t know. I am sure that I would have been more irritated than Nyitur was. Everything rolls off her back. She laughed when she told me the story again this week. “They didn’t believe me that I needed to stay! I knew my baby was coming. I am happy she wasn’t born in Susan’s car!”
Once I asked where Nyitur was born. With a big smile and told me that she was born in a field in Sudan by her grandmother. So much has changed for Nyitur in just one generation. I wonder how her daughter will be treated in the birth room. Research has demonstrated a disparity among immigrant and native-born mothers. “Black immigrant women—mostly from African and Caribbean countries—who arrived in the United States as adults enjoy better birth outcomes than native-born African American women.” (Tiffany L. Green, “Black and Immigrant: Exploring the Effects of Ethnicity and Foreign-Born Status on Infant Health” )
It doesn’t stop with the birth. It’s harder for African-American women to receive postpartum care than it is for white women. Regardless of race, it’s difficult for some women to seek support after having a baby. Mental health can be stigmatized. New mothers don’t know what is normal. In this frightening article written in the New York Magazine “Do I Really Want to Hurt My Baby?Inside the disturbing thoughts that haunt new parents.” a woman, Emilia struggles with intrusive thoughts. She thinks about harming her baby. She lives in fear of admitting her truth. She has no idea her thoughts were common and could be treated. She finds help and feels better. Her story shines a light on a huge problem in our country with postpartum regardless of race.
Postpartum mood disorders are real. One in five women suffer some degree of depression, anxiety, OCD, bipolar or even psychosis. And then, for people of color… imagine the additional stigma preventing them from seeking help. NPR reported on Morning Edition November 29, 2019, that "the black community don't know postpartum," as one woman put it. "There's this expectation on us as women of color that we have to be these superhero strong, that we're not allowed to be vulnerable."
We have a lot of work to do to bring health equity to this country. It’s not just in the maternal world. You are probably seeing these sickening COVID statistics:
· 36% of coronavirus deaths recorded in Wisconsin have been among blacks, though they comprise just 6.7 % of the state’s population.
· 71% of fatalities around Memphis, Tennessee are Africans Americans, who make up half the population.
· 56% of Chicago’s deaths have been African American, though they make up just 30 % of the city’s population. (African Americans struggle with the Disproportionate COVID Death Toll, Rodney Brooks)
Chicago’s Mayor Lori E. Lightfoot said the numbers are “troubling” and “a stark reminder of the deep-seated issues which have long created disparate health impacts in communities across Chicago.” There are so many issues: health, socio-economic, poverty, education and systematic racism. But as highlighted in the Brooks article, “it’s the healthcare disparity that’s driving the epidemic.”
I ask myself: what do I do with this awareness?
What is my action?
In 2018 when I read the New York Times article, I was in the midst of earning my doula certification. I felt hopeful when I read that being a doula can be part of the solution. Doulas are advocates for mothers. Doulas witness the birth and can potentially minimize tragedy. Dána-Ain Davis, the director of the Center for the Study of Women and Society at the City University of New York, said in the Times article that “at the point a woman is most vulnerable, she has another set of ears and another voice to help get through some of the potentially traumatic decisions that have to be made.”
My volunteer work at the University of Utah has provided me opportunities to support women of color. I think about my friend Rose Marie who was African and alone in her birth room. I am so happy I was there for her birth. I am inspired to do more. The world needs more doulas. And doulas of color. I am going to work on that.
As for the rest of the health care system, I, like you, wait anxiously to see what change the “great pause” brings. Race is hard to ignore when the data is right in front of us. Let’s talk about these issues even if – especially if – they make us uncomfortable.
COVID-19 present us with new opportunities. The question is not whether the post-pandemic world will be different. It is how. I hope that we move towards more health equity. We will see.
The Day of Grey
At 4:00 a.m. on March 6th, my phone rang. My husband nudged me. I am a sound sleeper. We both immediately knew why my phone was ringing. A client was in labor. I shuffled to my phone, but not quick enough. I missed the call. Eyes blurred with sleep, I read a text from my client’s husband written two hours previously: “Game Day.” His wife’s contractions had started. They were three to five minutes apart and a minute long. When I called him back it went straight to voicemail. He followed up with a text saying that they were at the hospital. She was 90% effaced and 4 centimeters dilated. Active labor had begun.
Forty-five minutes later I entered the double doors of Park City Hospital’s Labor and Delivery floor. Calm energy filled the hospital room. My client was on her hands and knees contracting. She met every contraction with a deep breath and laser focus. Her husband rubbed her back, whispering words of encouragement. I jumped right in, starting by squeezing her hips. I provided physical counter pressure and emotional support through every contraction.
My client had planned for an unmedicated birth and so far she was on track. She calmly contracted with her eyes closed. Her strength was inside her body. She breathed. She moaned. She stayed focused on opening her body and letting the contractions flow over her like a wave.
Dawn arrived. Orange sunlight filled the room as my client’s labor intensified. When her back ached, I pulled out my Robozo, a Mexican wrap, and tucked it under her pregnant belly. I gently shifted the wrap back and forth to bring her comfort. I offered a bath and snack. Neither sounded good. She felt sick. She threw up, as is common in labor. At one point, her nurse offered liquids through her IV and she wisely agreed. With more hydration, she felt better. And when the nurse brought an orange popsicle, that helped too.
My client was kind and polite. She never forgot her manners. She graciously thanked us. She did not complain. She smiled when she could. She was a pleasure to be around.
One of my jobs as a doula is to remind my clients to go to the bathroom and change positions during labor. Climbing out of bed and walking to the bathroom forces movement. Movement helps labor progress. My client’s favorite position was hands and knees - until her knees needed a break. She moved to the “throne position”. We rearranged the hospital bed so the back was tall and the foot of the bed low. Like a queen, she up in the bed and I pushed on her knees for comfort. Occasionally, we mixed it up and she stood swaying or sat on the birth ball. No matter how her body was positioned her contraction ritual was the same. She felt the sensation building, paused, took a deep breath, closed her eyes, and coped.
Her dilation was steady. When I arrived at 5am, her cervix was dilated to 4 centimeters. A couple hours later it was 4.5 cm dilated. Typically, a nurse checks a patient’s cervix every two hours in labor. When it was time to be checked, my client declined. She chose to labor without interruption. Three hours later when she was checked she was dilated to 7centimeters which was tremendous progress.
It’s tempting for a laboring woman to want to be checked every chance there is. Naturally, they want to know how close they are to the end. However, when my client declined a cervical exam, it kept her in a zone. She remained in her body rather than in her mind. Laboring women who can turn off their thinking minds progress more rapidly. I saw that principle in action.
Around noon, the doctor arrived at the hospital and checked her cervix. Since there had not been any progress in an hour and half, he suggested to rupture her amniotic sac. Breaking her bag of waters allowed the baby’s head to apply more direct pressure on the cervix and encouraged dilation. She agreed. Moments later, amniotic fluid gushed out, marking the beginning of the end. Her contractions intensified. They were sharper, closer to together, and longer. She stayed focused using her breath, vocal chords and determination.
An hour and a half later, at 1:30pm, she felt pressure and was ready to push. Her nurse checked her cervix again and declared her “complete” which means she was fully dilated to 10 centimeters.
The doctor came back in and the room was set up for delivery.
With every contraction that followed, she pushed. It only took a few rounds to figure out the most effective way to push. She was a quick learner. The baby’s heart rate dipped. This is not unusual, but the doctor asked her to relax through a contraction. The four-minute break gave both mama and baby a chance to regroup. The next contraction the baby crowned. Excitement filled the room when we saw that he had a full head of hair.
Motivated now, my client pushed one more time and at 2:15pm on Friday, March 6th, her beautiful baby boy was born. They named him Grey Charles.
Grey was quiet at first until the doctor suctioned his nose and mouth, and then he gave a big cry. Emotion filled the room. Tears filled my eyes. A birth! A brand new baby was born.
Birth is always amazing, but this one was especially beautiful. It was such a pleasure to witness my client’s plan come to fruition. Her body started labor on its own which helps avoid intervention. She coped with the contractions using her breath and focus. She met each contraction one at a time. She never doubted herself. She knew what she wanted.
My client sweetly texted me the next day: “Thank you so incredibly much for an incredible, positive, loving and empowering birth experience!!”
I love this work! As I proceed on my journey of birth education and doula support, I will remember this birth and the power of the mind.
Time of Zwischen
One of my best friends Erika, who’s half-Columbian, told me once about a Spanish word that names the last morsel of dessert/appetizer/food that no one ever eats: the single piece left alone on a plate. When offered, we say, “No. Thank you. I am all set.” Even if we want that last bite, we are too polite. The phrase is el de lavergüenza. It translates to “the piece of shame”.
I love a word that says it all.
I read an article by midwife Jana Studelskacalled The Last Days of Pregnancy. She writes about a place of “in between” which Germans call “zwischen.” At the end of her patients’ pregnancy, Ms. Studelksa’s tells the tense and uncomfortable almost-due mamas that they are in the “Time of Zwischen.” She describes this as a place “where the opening begins.” She believes that by “giving it a name, it gives it dimension, an experience closer to wonder than endurance.”
Anyone who has experienced the last days of pregnancy can attest that these hours, days, even, sometimes, weeks can be brutal. Especially when our baby does not arrive on our due date (which, I teach as“due time” because only 5% of babies are born on their due date.) There is so much expectation around a date. Couples attach to that day and then inevitably are disappointed when they have to hurry up and wait. Practicing patience at the end of forty weeks is the worst.
However, as Ms. Studelska writes, this time is not just biological, it is physiological. Mothers are preparing for the birth of a baby, but they are also preparing for their own birth: the birth of a mother. Both her body and her soul need to ripen and open. A relaxed, confident mother is inevitably going to be more comfortable than a tense and frustrated one. Those tightening emotions work against softening and opening. By naming this space - the Time of Zwischen - we honor and reflect upon the world-as-we-know-it, before it changes forever.
I am working with a client who is expecting any day. She’s mildly contracting and beginning to dilate. Her best friend from Oregon came to town to spend the last few days with her before the baby arrives. They came to the OMazing studio for a yoga class. Watching them on their mats, practicing next to each other was a beautiful sight. Their love was palpable. They smiled retelling the story of how her friend said to my client the night before, “You know what you need to do tonight? Dress up and go out with your husband on a date. Just the two of you. I’ll stay home and you two enjoy each other.” Agreeing, my client showered, slipped a dress over her enormous belly and went out with her husband. They had a great date: likely the last one before their baby will be born.
Never knowing when a women starts labor, we all want to know how to know when it is the real thing. I teach in my childbirth classes, that a woman is in “real” labor when her contractions have an established pattern. Couple are encouraged to labor at home as long as possible. The University of Utah hospital recommends that couples arrive after a contraction pattern of 3-1-1 (contractions have been 3 minutes apart, 1 minute long, for 1 hour.) When couples arrive too early to the hospital, the labor can change. The bright lights, interruptions, and distractions of the hospital might actually stall or delay labor. This delay, in turn, can lead to a higher chance of interventions or a longer labor. And if she is not dilated enough, the couple could get sent home - disappointing and tough.
I teach expecting parents how to plan out their early labor. I want them to do what feels good: rest, bathe, walk, bake, or watch a movie. I teach them techniques to cope with the early sensation in a calm and relaxed way. The longer the couple stays at home, the more likely their labor will progress despite their location. However, it is hard, so hard to wait. Our culture is not very patient, and waiting for the baby can be maddening.
I believe if we shine a light on these last days of pregnancy, the Time of Zwischen, women will know more about what to expect. Maybe the end will be less arduous and sweeter. Early labor is a spiritual transformation and not on a time table. Surrendering control is a practice and early labor is great place to start. As soon the baby arrives, we parents discover the truth about control. We have very little.
Guest Speaker @ the HIVE launch
January 14th, we kicked of our Hive Family Collective speaker series. We nailed it with the weather. Or more accurately, the weather nailed us! An epic Park City blizzard rolled in an hour before launch making it nearly impossible for most to attend. A few brave souls made endured the gnarly traffic and roads closures. My friends and fellow Hive founders, Perry Hardy, Joanna Kahn and I were the guest speakers. We introduced ourselves and shared reasons compelling us to be involved in this passion project. Here’s my story:
I have two insights for you today: with mindfulness and awareness, we can affect our thoughts AND you are not alone.
I’ve learned over the years that my reaction to a situation is my choice. It’s sometimes easier said than done. Growing up, I’d experience an emotional event and often respond thoughtlessly by yelling, swearing or even slapping something in frustration. Yikes.
At some point, I realized that I had agency over my behavior. I didn’t have to act that way. When I took a breath I had more space to choose a reaction - I was way more calm. I felt better. I know that I am not in control of the universe. But I am in control of my thoughts.
The birth of my son illustrates my point.
I am Sara Hutchinson and I am honored to be here today as a co-founder of Hive Family Collective. I am a certified doula, yoga instructor and childbirth educator. I’m a proud mother of two really good human beings. My daughter, Sadie is a middle school preteen and my son, Brewster, is fifteen.
My parenting journey has had it’s share of ups and downs. It looks more like the hills of North Carolina than the flat roads of Iowa, but I am enjoying the ride.
Fifteen years ago, I left my job and best friends in San Francisco and moved to Park City with my husband, Matt, seven months pregnant. The California hippie in me sought out a twelve week Bradley method childbirth class. If are not familiar, the Bradley method it is a wonderful, intense deep dive into childbirth education. For twelve weeks, my husband and I sat cross-legged on the floor and learned about breath, nutrition, and ways to cope in labor without medication.
Our lovely knowledgeable instructor was extremely crunchy, Her toddler would walk over and hop on her lap, life up her shirt and start breast feeding. They clearly were honoring the process of letting the child nurse until they both were ready to ween but it was an eye opening experience to watch.
I was pumped for my birth. My doctor told me at my last appointment that the baby’s head was down in good position. Two days before my boy’s birth-day I experienced hours of labor which goes down in this story as a false labor. After contracting all day, they sensations stopped and didn’t start up again until Sunday afternoon. Around midnight, we drove down Parley’s Canyon in a snow storm and pulled into St Mark’s Hospital. Excited and nervous like all first time parents, we checked in. A nurse checked my cervix:
“That is not a head down there.” The nurse said.
“What?” I said breathing through the sensation.
“That’s not a head. You know what that means?”
“No! I don’t know what anything means.” Annoyed.
“C-section.” Her sing-songy voice imprinted in my memory forever.
“No way.” I responded in disbelief. “Can I stand on my head? Go to a pool and do summersaults? Acupuncture?” I was desperate.
“There is nothing you can do now that you are in labor. Your doctor is on her way.” 15 minutes later they rolled me into the OR and pulled out my beautiful boy Brewster.
Here illustrates a valuable lesson: Do not attach. It might cause pain.
If I had brewed on the fact that I had to have a cesarean section, I would have missed out on the joy of his birth and golden hours which were perfect for me. Not on paper. Brewster was whisked away and put under warmers for a few hours leaving me alone. But I dug deep and focused on the positive and the big picture. My positivity saved me.
My mantra is to make plans and remain flexible. Yes, I wanted an unmedicated birth. Yes, I had a c-section. It was what it was…..
Still, I was the happiest new mama on the labor and delivery floor. Looking back, I know the joy was inside of me. Nothing could have dimmed my light.
My reaction to my birth outcome was a choice.
I have choices in my life every day. Some big, and some small. Last year, I chose to go on a sabbatical last year in France with my kids. That was a big one. And when I returned to Park City I had another choice to make. Rather than finding another office job, I started OMazing Birth. Not as predictable but soul-filling. I love working with women preparing their bodies and minds for birth and the transition to parenthood.
I think of birth like the wedding and parenting is the marriage. Our role as moms and dads starts on the day the child is born which is insane. But with a splash of mindfulness and intention and a few good friends, the journey can be smoother and more fun.
Raising kids is both exhausting and tremendously rewarding. Why not do it in together? So many of us live her in Park City without out best friends or family. Hive Family Collective exists because we are better together than we are alone.
Thank you for showing up tonight.
Myself, Joanna Kahn & Perry Hardy Live at Hive!
New Beginnings
I wrapped up 2019 sitting on my living room couch next to my husband. We watched Tina Fey and John Slattery brilliantly act in an episode of Modern Love - an Amazon Prime series I highly recommend. I needed to stay awake. My teenaged son was at a New Years party and I told him I’d be his Uber at 12:30. The Modern Love drama helped me keep my eyes open. Mid-episode I noticed on my phone that it was midnight. I texted my eleven year-old daughter who rung in the New Year with her cousins. I was happy that she responded as she had a clear goal of staying up this year. We exchanged a slew of emojis and I know she went straight to bed. At 12:20am, when the show was over, I headed out to pick up my boy. TwentyTwenty had arrived.
I like the ritual of new beginnings. I welcome a chance to reflect on the year past and reset in a new year. My 2020 intentions are clear. Invite joy, peace and calm into my everyday life. I am using Miguel Ruiz’s four agreements as my guiding principles: Be impeccable with your word. Don't take anything personally. Don't make assumptions. Always do your best.
I feel fantastic about my 2019. Starting OMazing birth was a leap of faith and I have enjoyed every step. It’s still in its infancy but growing slowly. This next year, I will teaching more, assist more mamas and create new programs.
One of the most exciting partnerships is with my friend Perry. She gave birth to her second baby this summer. Mom of two, she struggled with all things new-mom: the shifting family dynamics, returning back to work, noticing how little time she had for herself. Even though Perry has a tribe of like-minded friends in similar situations, she felt alone. Convinced that she was not the only one going through these milestones she wondered, where was everyone? Where is the support?
She looked to a program that her sister-in-law started in Bozeman, Montana called Roots Family Collective and realized that Park City needed something similar.
Perry and I met in November to share ideas and it was magical. We continued to meet every few days for the next six weeks. We talked with friends and professionals all over town: health providers, Community support liaisons, and of course friends. Every person we shared our ideas with enthusiastically supported us. Perry is very committed to this mission and I am excited to help.
Late December we named our organization: Hive Family Collective. We committed to hosting a speakers series once a month: the 2nd Tuesdays of the month from 4:30-6pm. Perry found space at our local hospital and created a flyer. We are booked on our local radio to talk about our first event next week. Hive is happening!
Just like OMazing in 2019, Hive is a 2020 intention. We planted the seed. We made a plan. We will execute. We start small and grow. This new beginning lights me up!
What is your intention for 2020? How can you make it happen? I encourage you to take a moment to name your intention. Focus on it. Love it. Watch it come to life.
Thankful.
Who doesn’t love Thanksgiving? A five day break from the the office and school that revolves around a gigantic meal is welcomed every year. The focus on family, friends, pie and gratitude makes it not only a heavenly holiday, but my favorite one.
Gratitude is the highest vibration. I know that to be true. When my heart is full of appreciation, my existence is more peaceful and joyful. Perspective grounds and centers me. I am healthy. I live in abundance. I work with women preparing and giving birth. What gifts!
The Tuesday night before Thanksgiving, I volunteered at the University of Utah hospital as a doula. It was hard to leave my family after dinner. My daughter gave me her pouty face. I was tired. However, I knew that once I arrived on the Labor and Delivery floor at the hopsital, I’d wake up and would not regret being there.
I arrived around 9pm and checked in. The charge nurse sent me to Room 2. A twenty five year old woman, Maria, was seven centimeters dilated and struggling with her contractions. She was waiting for an epidural and was climbing the walls with every surge. After a quick introduction, I started pressing on her hips offering counter-pressure. She was using Nitrus for relief but her contractions were coming on top of one-another. It was intense. I knew that my assistance was appreciated but we were all business. About thirty minutes later, the anesthesiologist arrived and administered an epidural. Maria’s pain was instantly relieved and she closed her eyes.
I love choices. I wholeheartedly support any decision a birthing woman makes in labor. The birth is her experience. Prior to labor, whether in a yoga class or childbirth education class, I share benefits about moving around in labor. It often helps the cervix dilate quicker. With an epidural, the relief of pain is divine, especially if a woman has been in labor for hours and hours. But it can stall labor and dilation. The body is relaxed and there is no gravity helping the pelvis open and the baby move down. And a stalled labor is what happened with Maria.
Right after the epidural, she immediately fell asleep. I tip-toed out of her room and went back to the nurse’s station. I checked in with the charge nurse who sent me to Room 12. I met a couple who was having their second baby. Kate, the mother had been induced a few hours before and was waiting for her epidural. She had no desire to labor without medication so she was just killing time. I sat and chatted with her for an hour or two while her contractions started. When the anesthesiologist came in to administer the epidural, she asked her fiancee to take a photo. The nurse asked if he was comfortable with seeing the needle in her back and he said he had no problem with needles. His body was covered in tattoos so we all had a laugh and agreed he had seen many needles over the years.
We were wrong. This guy was not OK. Right when the doctor was placing the needle in Kate’s spine, the fiancee said, “ I am going to pass out.”
And he did! He sat down and lost consciousness right next to the hospital bed. I stepped closer to Kate who had to sit still because of the epidural. I assured her that he was OK and she needed to breathe. The nurse gave the father of the baby some juice and helped him to the couch.
“Well, I guess, I am not as tough as I thought,” he said in a self deprecating tone. Everyone in the room laughed. I reminded them that this was all just part of their birth story.
At around 1am Kate was medicated and ready to rest. I said good bye and went back in to Maria’s room. There were six family members crowded in the room silently watching the TV. I pulled up a chair next to her and asked her how it was going. She told me had gone from a 7cm dilation to a 6. She admitted she was very happy and comfortable. I sat with her for a few more hours. We talked and I supported her through any sensations that she experienced despite the epidural. She told me that she and her husband met in Mexico and moved to California and then Utah. They married at eighteen years old and wanted to have a baby from day one. It took them seven years to become pregnant. She gave up and didn’t think it was going to happen. And one day it did! She was so grateful for this baby girl.
Maria was a beautiful, strong woman. I know that she will be a loving mother. She was looking forward to Thanksgiving with her new little family. It was 5am when I said good bye. I hoped that I would have been present to support her through the birth, but there was a massive snow storm on its way and I was tired. The news was calling the storm a Bomb Cyclone. I drove home in the beginning of a blizzard and crawled in bed right before 6am.
I thought about Maria all weekend. The next time I am at the hospital, I am going to seek out her nurse and ask about Maria’s birth. I imagine that she had her baby Wednesday morning in the storm. The next day was Thanksgiving. Like me, Maria would have looked at her family and her heart would be filled with gratitude. We are all the same.
Thanksgiving = GivingThanks.
Awéé’: the Navajo word for “baby”
I met Karen on Monday morning in Room 11 on the labor and delivery floor at the University of Utah hospital. I introduced myself and told her I was volunteering as a doula. “What’s a doula?” she asked. I replied that doula translated to “servant” in greek. I volunteered at the hospital supporting women in labor. I explained that I offered physical and emotional care, but not medical advice. I breathe. I massage. I bring in my positive energy and knowledge to the room. I witness birth.
“Would you like to me stay?” I asked. She nodded. “Yes. I’d like you stay.”
Her husband, Dan, sat on the couch and smiled. He didn’t say much. They were both very quiet. But not their seven year-old daughter, Teagan. She and her cousin filled the room with all the conversation needed. Excited for some fresh energy, Teagan peppered me with questions like, “What is your favorite animal ?”
“Polar bear” I replied with a smile. She reminded me of Sadie, my eleven year old daughter.
My conversation with Teagan was quick because her mom was contracting. I watched Karen take a deep inhale and close her eyes. She handled early labor calmly and with focus. I walked over to the side of the bed near her head. Quietly, I reminded her to relax her shoulders, jaw and fingers. After the contraction, I complimented her and offered her a sip of water. I noticed that throughout the entire contraction, her husband didn’t look at her. Preoccupied by the TV and his phone, he did not comfort Karen. She was basically alone.
I noticed that the word “unmedicated” written on the white board in her room. Intention set. Before the next contraction, I asked how labor started. Her water broke the night before and she didn’t contract much until arriving at the hospital at about 8 a.m. She was happy that her body naturally went into labor as the doctors were planning on inducing her the following day. Her due date wasn’t until the first week in November.
I asked myself: WHY?! Why all the indications at 39 weeks? Not knowing any of her medical background, I don’t know the reason. However, I am confident that were she induced, an unmedicated birth would be much more difficult. Not impossible, but likely more intense, and likely to lead to a cascade of interventions.
Karen was dilated to three centimeters when she was “checked” by her nurse at 11am. Agreeing that she was not progressing quickly enough, the nurse administered pitocin. Pitocin is a synthetic drug that acts like oxytocin, the hormone needed to contrast a woman’s uterus. With pitocin in her system, Karen’s labor intensified. She continued to handle each contraction methodically with breath and focus and my reminders to relax.
Around noon, Dan talked his brother on the phone. He was on his way to pick up the the little girls. I didn’t recognize the language Dan spoke. I asked Karen what it was. She told me that they were speaking in Navajo. “Are you Navajo?” I asked. She replied “Yes".
Cool, I thought. I am supporting a Navajo family. This is a first.
When Dan’s brother arrived, he didn’t say anything. He stood at the door and the girls scurried out of the room. Neither Karen nor her daughter said goodbye. Wow, maybe she is not like my daughter? Sadie would be ALL over me. A couple of hours later, Karen’s sister arrived and she walked in the room without acknowledging Karen. It was twenty minutes before they spoke. I think I was the only one who found this unusual.
Was their behavior cultural? I have nothing to compare it to. I can only imagine how the attention I gave Karen must have been over the top compared to what she was used to. Every contraction that she experienced, I reminded her to breathe and relax and I told her she was amazing. I know as a doula what kind of support is effective for a laboring woman: consistent and positive.
Karen’s labor was tough! She vomited, shook, and cried - all normal. I wrapped her in warm blankets and reminded her that her body knew what to do. Her transition from Stage 1 to Stage 2 of Labor - dilation to pushing - was textbook. She wanted to give up. She said she couldn’t do it. At one point she said that she begged for pain relief. The nurse told Karen that she could have whatever she wanted. However, by the time the anesthesiologist arrived, the baby might be here. Karen was close to the end. I appreciated how the nurse left all the decisions up to Karen. She decided to just keep going.
At 4 p.m., she said she felt like she needed to push. Dr. Clark, the OB on call was down the hall at the clinic and came into her room right away. She checked Karen’s cervix one more time and announced that she was “complete” meaning she was 10 centimeters. We arranged ourselves around Karen. Dan stood on her right side holding her hand. He was so sweet, whispering in her ear. Her sister stood next to him and I was next to her. A medical assistant and I held her legs back as Karen pushed. It was hard for me to hold on to Karen’s leg. She’s a strong woman. Holding the leg of a pushing mama who is not medicated is so different than a mama with an epidural. It’s like comparing the force of a gorilla to a monkey.
With every push, the baby moved down the birth canal. Karen only pushed for 10 minutes and her daughter was born.
I witnessed another miracle. Karen delivered her placenta without issue. The doctors told her that she did not need any stitches. She would be sore, but would heal fast. I have noticed in the past seven months of supporting births that women who chose an epidural generally need stitches. I have been thinking how the intensity of the pain of birth might be delayed by choosing an epidural. With an epidural, a laboring mama skips the intense pain during the labor, but the intervention of an epidural might lead to a more difficult birth. With a good epidural, a mom doesn’t feel much when the baby is delivered so there may be more intervention at birth which could lead to stitches in the vagina causing longer-lasting damage. I haven’t seen data, but this scenerio is on my mind.
When I said good-bye to Karen, she looked me at me intently. “Thank you.” she quietly said with her baby on her chest. “I couldn’t have done it without you.”
I told Karen that it was an honor to witness such strength. Her sister hugged me. With tears in her eyes, she too thanked me. I felt so much love in Room 11. A new awéé’ in the world!
Reflection: Sadie's BIRTHday
My daughter Sadie loves to hear about the day she was born. “Tell me the story when you cried because I was a girl.” I laugh. “Sadie, I would have cried regardless if you were a boy or a girl. I was so happy to have a baby.” But Sadie is right. I REALLY did cry when they announced that she was a girl. I was just so surprised.
Today is Sadie’s birthday!
Eleven years ago Sadie arrived via cesarean section. I didn’t know her gender so I assumed I was having another boy. My heart pined for a daughter but my mind didn’t allow the attachment - too much. I love boys, and if I had a second boy, I know that brothers have a special bond. But in my heart, I wanted a daughter.
My mom convincingly told me I was carrying another boy. “Oh Seera, you look the exact same as you did when you were pregnant with Brewster. ” My mid-western mom says my name with a strong Chicago accent. Hindsight twenty-twenty, I looked the same because both of my babies were breech - folded in half with their head and feet up and butt down. Very yogic.
It was news to me in 2004 that my son was breech. A few days before his birth my OB told me the baby’s head was down. A couple days later, consistent contractions swept over me and then my labor abruptly stopped. Two days later, I contracted again. This time my labor was real. Did my son flip in my false labor or if my doctor called it wrong? I still wonder.
I showed up at the hospital at 1am and a nurse checked my dilating cervix. She smuggly said,. “I don’t see a head. You know what that means?”. Contracting, sweating, overwhelmed, I said. “NO. I don’t know what that means. I know nothing, this is my first baby. “ I could have smacked her.
In a sing-songy voice she said ““SEEEE-Section.”
Shocked, I tried to digest that I was not going to have an unmedicated birth. Our twelve weeks of Bradley natural childbirth education would not be useful in the operating room. Disappointed and desperate, I begged for time to turn the baby. Could I stand on my head or summersault in a pool? Acupuncture? My requests were futile. It is nearly impossible to turn a baby in active labor. The good news was that my OB was near by. Being the holidays, her mom had just arrived from NYC. My doctor and her boyfriend picked up her mom at the airport and drove to the hospital. My doctor’s boyfriend and mom waited in the lobby while my son was born.
Flash forward, nearly four years later, my baby was breech again. I wanted desperately to turn her and try a VBAC (Vaginal birth after cesarean). Hypnosis, acupuncture and the magic of our local prenatal chiropractor had not worked. Our last attempt was a manual turn that had to be done in a hospital by a doctor. Despite having the reputation of being painful, I wanted to try. The day before Sadie’s birthday, my husband and showed up at the hospital for an ultra-sound. No dice. Like her brother she was frank breech. Her butt was down. Without legs to kick around, our only choice was another cesarean.
“Would you like to go back for surgery now?” My doctor asked after relaying the news. “ Yes.No.” Matt and I spoke simultaneously. Matt was ready. I needed a day. I won. We returned the next day for our planned cesarean. Walking in to a birth not in labor is both bizarre and calm. After a bunch of easy paperwork, they prepared me for surgery.
It only took about seven minutes from the beginning of the procedure to Sadie’s birth. The whole surgery takes under an hour. The doctors were so casual. The talked about the new iPhone as they pulled my baby out of my abdomen. I heard a cry. “Who is going to announce it?” One of the technicians asked. Pause. I was dying. Someone, speak! My doctor said, “She’s a girl. You have a daughter”. And Sadie is right, I cried. Oh, did I cry.
My husband called my parents who and my mom answered the phone with the hopeful question, “Do we have an Abigail?” (My mom loves the name Abigail and was not only hoping for another granddaughter, but one named Abigail) Slightly confused, Matt responded, “We do have a girl, but we named her Sadie.” He heard people in the background. Their conversation was short. Next he phoned call my sisters, KC and Mara to share our news.
Afterwards, we heard that KC called Mara and said, “Exciting. Sara had her baby! Did you hear that they named her Katie?” That would have been odd as Mara’s daughter’s name is Katie. Mara said “No, it’s not Katie, it’s Sabie. I looked it up and Sabie is a town in South Africa. Strange, don’t you think?” KC said, “I don’t know about Sabie. Let me call Mom & Dad.” KC called my parents and asked “What is the name of Sara and Matt’s baby?” My mom responsded, “I don’t know. We couldn’t hear. We have friends over.”
KC called Matt and asked what our baby’s name was because none of them knew. Matt asked me “What’s wrong with your family?” I laughed and said if we have a third, we would text them the name.
I love revisiting Sadie’s birth story, especially on her BIRTHday. What’s your story? Don’t forget to share it. Again and again.
The Birth Story of my friend, Rachel
I met Rachel last winter in a friend's kitchen. Pregnant with her second child, I was so happy to talk to her. I just crystalized the idea for my new business OMazing Birth and was excited to share my ideas and knowledge with anyone relevant. Rachel and I connected immediately. I invited her to be my prenatal yoga student and for the next few months, we practiced yoga together in my living room or at her house. Rachel's local midwife wrapped up her career in the middle of Rachel’s pregnancy and she was not sure who or where she was going to deliver the baby. But she loved her doula Robyn Carter and completely trusted her. Rachel felt confident that as long as Robyn was at her birth, she was would be fine. She jokes that the best thing that she ever did was marry her husband Justin. The second, was to hire Robyn! I completely understand as Robyn is my teacher, mentor and friend. She is the best!
I woke up on Labor Day and Matt (my husband) asked me if I had any work to do. “Labor Day, get it?” Ha….What do you know?? My phone rang later that day at 3:45p and it was Robyn Carter. She needed my help as she was stuck in Labor Day traffic. Could I go to the Park City Hospital to support her client, Rachel Bieber? “Yes, I replied! I know her and I’d love to help” I changed my clothes quickly and hit the road. I called Robyn back at twenty minutes later from the hospital parking lot and learned that Rachel was 8cm dilated and begging for an epidural. Robyn would be there shortly but I was instructed to go upstairs to the 2nd floor and look for the two nurses on call, Robin and Sarah. I smiled at our birth team: 2 Robins and 2 Sarahs.
When I arrived on the second floor I heard Rachel laboring and walked into her room. Rachel was draped over the back of the bed and Nurse Sarah rubbed her back. Her husband Justin held her hand and repeated encouraging and positive words with every contraction. Rachel was coping without any medication.
I hopped right in with my support. Justin gave me a quick hug, thanked me for coming and we went to work. Rachel knew she wanted pressure on her hips so I squeezed her hips. She was moaning, breathing hard and throwing F bombs, typical for a woman in transition. About 10-15 minutes later, Robyn walked in and Rachel was “complete” meaning she was 10 centimeters dilated and ready to push.
“How much longer will this take? I want an epidural!” Rachel said. The doctor on call, Dr Falk explained that the baby would be here before the effect took place and to hang in there. We turned Rachel over on her side and then back on her hands & knees. Rachel’s contractions subsided as her body took a break. For several minutes Rachel closed her eyes. It is natural for there to be a break in between the 1st and 2nd stage of labor (dilation & pushing) Justing wiped her forehead with a cool cloth and we waited.
Rachel turned over on her back and she felt extraordinary sensation. Robyn reminded her of her strength. I reminded her of her breath. Justin encouraged her to “get this done". Dr Falk patiently waited and rubbed oil on her perineum, something I have only seen midwives do. Oil helps to stretch the perineum to help avoid tearing.
Once Rachel had the urge to push she worked with her contractions and used her power to “bear down”. It wasn’t long before we could see her baby’s head and hair. At that point and for the next few minutes, Rachel gave all that she had and pushed. The sensations were intense. She felt everything and used her mindfulness to focus.
Her baby boy arrived at 5:15pm and immediately went to Rachel’s chest for skin-to-skin bonding. Rachel closed her eyes. She was exhausted and relieved. Nurse Sarah wiped the baby off and Justin asked to keep some of the white “stuff” on him - vernix is what is called. Justin cut the umbilical cord after it stopped pulsing. I over heard Justing tell his son that they would take good care of him which made me tear up.
The final stage of labor is delivering the placenta which Rachel did a little while later. Without any medication, this too was sensational. Robyn and I tapped her shoulders and reminded her that this was the end. She was no longer pregnant. Rachel did not have any tearing nor need stitches. I was truly impressed with how Rachel followed the intuition of her body to birth her baby boy. She stayed in the hospital over night and was home the next day. She said that Park City Hospital was a positive experience.
I visited with Rachel last week to meet Parker and check in with how she was feeling. Her recovery has been great although she is exhausted. Babies can confuse night and day making it hard to function in a world that sleeps through the night. I was really interested in how she ended up at the hospital since I thought she was planning a birth center or home birth.
She said that she had been going to the doctors in Park City for well-checks and had to really push back on being induced at 39 weeks. That is the protocol for her age and anyone over 35 years old. She knew that she did not want to be induced and was able to go to her due date. She was still considering a home birth with a midwife, but due to her intense labor she ended up at the hospital.
On Monday morning, the day her son was born, she hiked up the PC Hill which is pretty steep 45 minute hike. She came home and her husband wanted to go on a bike ride. She had a feeling that was not a good idea and asked him to stay home, and he did. It was a good thing because she started contracting. Rachel took a bath and the contracts became more severe. Laying on the bathroom floor, she told Justin to call Robyn, their doula. At that point, they decided they needed to go to the hospital and Rachel decided at that point she was going to have an epidural.
However, her body labored so quickly and so the story goes, there was no time for an epidural. Instead she had the support of two doulas, two fantastic nurses, a caring doctor and her loving husband Justin. It was all the comfort that she needed to birth her baby boy.
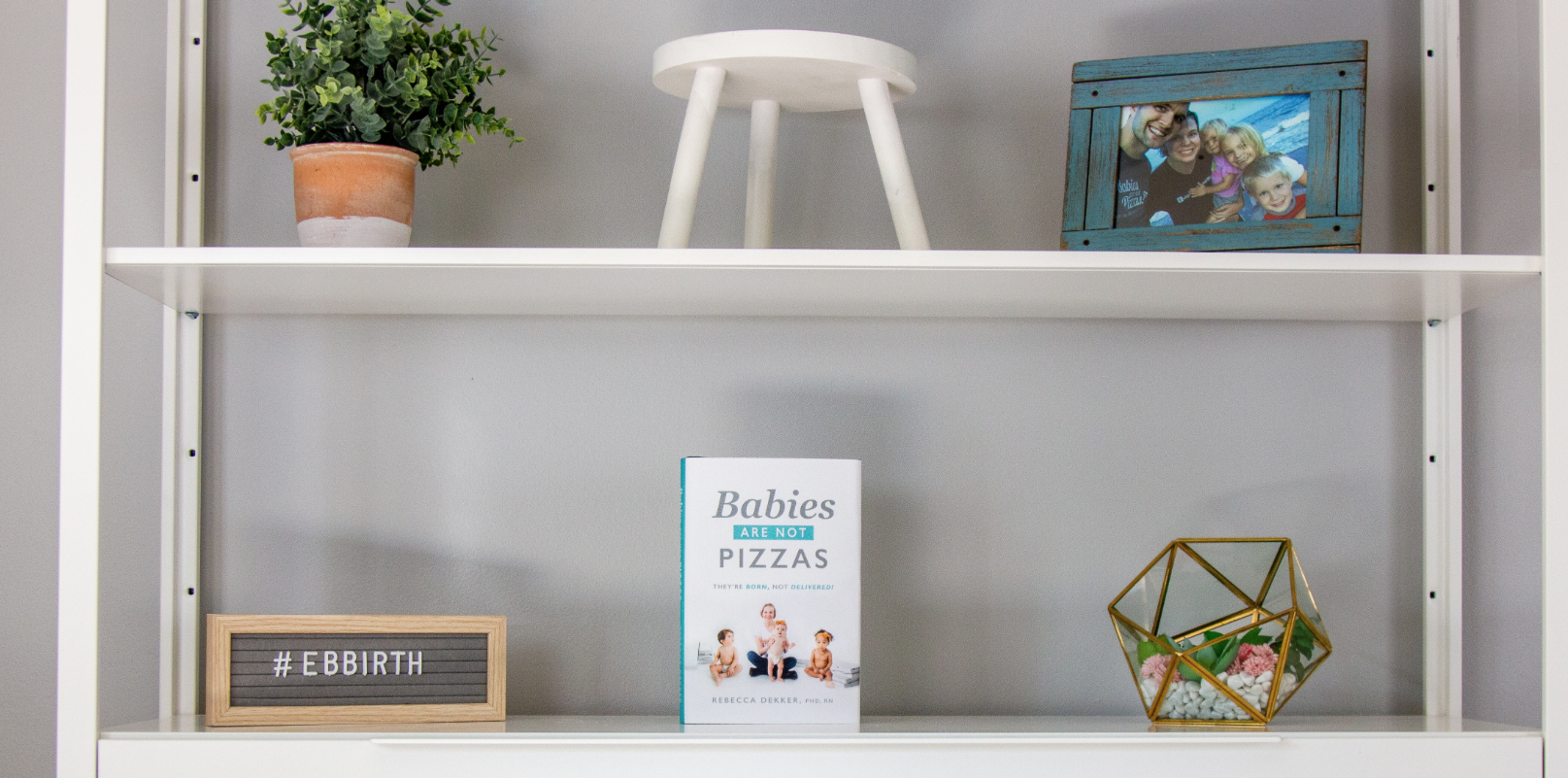
Babies are not Pizzas
One of my college roommates hosted a Bat Mitzvah for her daughter in New York City last weekend. I flew across the country with my two kids to attend the magnificent event. This was my first Bat Mitzvah. I was blown away! Starting with a three hour morning service at the Synagogue and ending with a six hour party on the Tribecca Rooftop in New York, it was a day to remember!
On the flight, I read Rebecca Dekker’s new book, Babies are not Pizzas: They’re born not delievered. Rebecca founded Evidence Based Birth, a “for purpose” company (as she calls it) after her first birth. Rececca admits that it took her a few years to realize that her first birth was traumatic because she achieved her goal of not having a cesarean and left the hospital with a healthy baby. However, her hospital birth was far from ideal. Many of her procedures and interventions were based on hospital culture and routine, rather than evidence. She wrote “almost everything that was done to me in my first birth had already been proven by research evidence to be either not helpful or actually harmful to healthy people who are giving birth.“ I read this and thought, what is going on? Rebecca started EBB with a mission to put accurate, evidence based info into the world to create positive change around birth. She is doing important work!
We live in a medicalized birth culture in the United States. Hospital administrators, doctors and nurses mitigate risks of an unfavorable birth outcome by controlling labor. When I volunteer at the hospital, I see it. Births are being dominated by cascades of interventions. An example is a labor can start with fear: mama is past due, she is over 35 years old, the baby is big. Those reasons can lead to an induction. Often to start labor, the mother will go on a synthetic drug called Piton which is admitted intravenously. The IV tethers her to the bed and the Pitcon creates intense contractions that are often not sustainable without an epidural. If that is path she is on, she will remain in bed until the baby arrives. With a laboring mama in bed, nurses can spend more time at their desk watching the labor on the screen, charting. Did yo know that nurses statistically spend only 6% of their time with a laboring mother?
I am not judging the decision of my sisters. My lady-friends. I get it. An epidural is not a bad way to go. It’s safe and necessary for some women and preferred by many. It can be a gift to birth a baby with out acute pain. I just wonder if medicated births are rougher? Is there more damage to a woman’s “downstairs” because a medicated mama does not feel the same sensation of an unmedicated birth? Will medicated mamas have longer lasting pelvic problems, incontinence or sexual dissatisfaction? I talked this over with a few friends at the Bat Mitzvah cocktail party and they agreed, yes. Maybe an epidural creates a pain-free experience at birth, but there are lasting effects that might not be as obvious.
I did a little google research and read One study shows that epidurals increase the risk of tearing. Another says that the reason more tearing occurs with epidurals is that more first time moms choose epidurals and first vaginal deliveries are already associated with a higher risk of tearing.
What else is out there? Rebecca’s book created a desire to study the data.
As a writer, I appreciate the back story of Babies are not Pizzas. Rebecca shared on her podcast that she started writing this book as a guide to pregnancy in 2017. The pages of her “how to” book were filled with evidence, interviews, and pieces of her story how she started EBB. After completing her first draft, Rebecca received feedback that the book felt disjointed and unauthentic. Taking the criticism to heart, Rebecca deleted her entire book and rewrote it as a memoir threading the evidence based research into the book. It took an additional eighteen months. Rebecca’s book exudes honesty and integrity. The humility and determination it must have taken to rewrite the book inspires me.
I am a big fan of Rebecca Dekker. She writes about creating change, sexism, raciscsm and being brave in our lives. And most of all she inspires me to study the evidence and share with my students and clients.
The End of Summer Brings an OMazing Beginning
My fourteen year old son confidently walked out of our house at 6:45am this morning to catch his school bus. He’d only been awake long enough to shower and eat a bowl of oatmeal. Typical teen, he didn’t say much, but I know he was ready for his first day of ninth grade.
His sister, on the other hand had a lot to say. Starting middle school has been on her mind for weeks and conversation has been non-stop. Before leaving for the 8:15am bus, she reviewed her schedule and locker combination, checked her school supplies in her new Jansport backpack, stuffed her lunch and swell water bottle in, and peeked in the mirror one last time. Her braids and outfit looked good. My daughter smiled, took a deep breath and said “Bye Mom. Bye Dad” . Her excited energy propelled her to the bus stop.
Going back to school is fresh. New teachers, classes, and maybe even some new friends . Each student walking through the door has a clean slate.
I share my kids excitement for new. One of the highlights of my summer was creating work space in my house. The OMazing Studio is open! I am so happy to a separate office to practice yoga, write and meet with clients. When my kids left for school this morning I walked upstairs to start my new chapter.
My desk and yoga space is separated by a sheer purple ombre curtain. I picked it out with my daughter. I laugh remembering her saying, ““You definitely need a curtain in case someone has a baby in the studio.” I looked at her sideways. “What?? They will need some privacy.”
She was dead serious.
I thought, we’d need a lot more than a curtain! In that moment, I knew that my daughter had neither an idea of how a baby was born nor how long it takes. To think my office studio would be filled with people and someone just might have a baby. Ten year old innocence is sweet.
I grateful to have a clean new space to call my own. I hope the soulful sculptures and green plants inspire me to accomplish greatness. I am excited to see how this OMazing journey plays out.
Thanks for following along!
Karla - So young. So brave.
I drove down to the University of Utah hospital after dinner last night. My volunteer shift started at 8pm and I met Karla, an extraordinary, young, and brave woman an hour later. Karla’s nurse invited me into her room. As a first time mama, she was interested in my doula services. I walked into a brightly lit room to find her two teenager siblings on the couch engaged on their phones. Karla sat up in the bed and graciously greeted me. Her gratitude shined brightly from the moment we met. “Thank you for being here. I am scared.”
Karla just turned 20 years old in April. Her sister was 15 and brother 18. He still wore his work uniform: a red IHOP shirt. He came straight from his shift to accompany his sisters. These kids were Karla’s support team. They had so many questions for me: What’s a doula? What does it stand for? How long until the baby arrived? How would Karla know when it was time to have the baby? Would Karla have the baby in that room?
They pointed to various equipment in the hospital room and inquired about how it was used. I quickly realized that I likely would be supporting this grateful young squad for the duration of Karla’s labor.
I quickly shared some basic childbirth education. I described the function of contractions, stages of labor, what effacement and dilation meant and how the birth may (or may not) unfold. The siblings lost interest way before Karla. She held on to my every word.
Karla was one centimeter dilated and had a cervical ripener called a foley bulb inside of her. We talked about birth preferences and she said she’d like to “go natural” but she was going to see how it’d go. I explained that really the choice was medicated (epidural) or not but either way she’d have a natural birth. (side note: I’d like to reframe this verbiage. Culturally, a “natural” childbirth means unmedicated, or without an epidural. But having an epidural or a cesarean section is not “unnatural”. It is just medicated.)
I wasn’t there long before Karla’s contractions picked up. Closing her eyes, I encouraged her to breathe deeply and trust her body. I massaged her shoulders, her feet and offered her water or ice after each contraction. Every thirty minutes or so I suggested a new position to Karla in hopes for some comfort.
I told her she was amazing. I told her she was brave.
Around 11pm, the foley bulb fell out and she was four centimeters dilated. Her contractions intensified. I implemented Penny Simkin’s 3 R’s (Relaxation, Rhythm, Ritual) and gave her counter pressure on her hips, knees or hand. Occasionally she reached for her phone and checked in with her friends. She told me that they were telling her to “get the epidural already”. She knew she didn’t want it, but she asked me how bad the pain was going to be, as if I had a crystal ball. I encouraged her to focus on one contraction at a time.
Around midnight her older brother arrived. He looked like a deer in headlights. He had never been around birth so he too had a slew of questions for me.
At 2am , Karla’s midwife checked her cervix. She had progressed, but only one centimeter, to a five. Karla didn’t hide her disappointment. She questioned her ability to do this without an epidural. The University of Utah is the only hospital in the state that offers Nitrus Oxide, so I encouraged Karla to try it. She agreed. The gas took the edge off of the contractions, but only minimally. However, it did buy Karla some time.
The midwife checked her cervix again an hour later and she was still at a five, with greater effacement. The next few hours were brutal. Karla continued to change positions. She stood and leaned over the counter. She sat upright in the hospital bed with her feet down in the “princess pose”. She laid on her side. With each contraction, she closed her eyes and tried hard not to fight the sensation with her moans and breath.
The girl was worn out. And sick.
Karla vomited several times. She shook. I assured her it was totally normal. By 3:45am she wanted to quit. For temporary relief, the nurse offered her a dose of fentanyl, a narcotic that takes the edge off the contractions for a short time but does not numb her body like an epidural. She was becoming desperate so she tried it. It helped her relax in between contractions but as promised, the effects did not last for long.
Fifteen minutes later, Karla declared she wanted an epidural. The anesthesiologist came in and routinely gave Karla the information about the procedure and side effects. She looked at me for approval. I reminded that it was HER birth journey, and there was no right or wrong way. I reminded her that an epidural is safe, and would provide total relief. Since she needed rest and was in so much pain with each contraction, she agreed and signed the paperwork. Moments later, the nurse said that that Karla’s midwife wanted to check her before she would have an epidural.
“No problem,” said the anesthesiologist. He continued to prep for the procedure. Karla’s midwife gave her a cervical exam and calmly said “Karla, you are a nine”. Karla’s eyes widened and filled with tears. “Really, a nine?? I am almost in labor?” Her nativity touched me. The midwife kindly responded, “You are in labor now but when you are ten centimeters you will be ‘complete’. Your cervix will disappear, and it will be time to push. You are very close.” I appreciated that the midwife then said, “You are welcome to have an epidural if you wish. It is up to you.” Karla looked at me. “What do you want?” I asked. “I want to do it without it. Can we say no for now?” Of course! I looked straight into her eyes and reminded her how amazing and strong she was, and that she was going to meet her baby girl soon.
With this news, Karla had renewed energy and determination. She managed each contraction with breath and focus. And by 4:45am, she proclaimed she was ready to push. The midwife checked her and she still had a little cervix intact, so with a hook the midwife ruptured her membranes (broke her water) which often speeds things along. Ten minutes later, the sensation to push was back, and Karla was complete.
The nurse paged the pediatric team who attend births in case there is an issue with the baby. I woke up Karla’s sister and laughed when Karla said her brother could keep sleeping. With the lights still dimmed, the team assembled. It was go time. Karla grabbed the back of her knees, I held one leg and the medical assistant held the other. Karla pushed to the count of ten with each contraction.
Four contractions and twenty-six minutes later, Karla’s baby girl was born at 5:26 AM. Karla sobbed “I did it!” She was so proud of herself, along with every person in the room. She truly dug deep and her strength never wavered.
The next thing she said was to me. “God bless you. You are an angel.” It was my turn to tear up.
The baby girl arrived into our world with little fuss. The nurses placed the baby on Karla’s chest for skin-to-skin while her little sister cut the umbilical cord. The pediatric team never even touched the baby. Karla did not need stitches which is remarkable for a first time mother.
I know Karla may have birthed her same healthy baby with or without medication, or me at her side. However, I am confident that my doula services helped her achieve her “natural” birth, which she was so proud to have accomplished. Her bragging rights and deep satisfaction will be with her for years to come.
Amazing work sister!
Birth Story: Mama of Six!
Doulas write birth stories to document the details of a birth. We are observers. A birth story can be a gift to the couple who may or may not remember the details of the birth. Fourteen years ago, my doula wrote me a card with details that I barely remembered from my son’s birth. True treasure.
The following birth story is from a birth in April. I supported an incredible woman from Tonga on a volunteer shift who birthed her sixth baby. Her oldest child is eight years old.
————————-
I arrived to my volunteer shift at the U of Utah at 8:30 am on a Tuesday morning. First order of business is to check in with the lead charge nurse. I asked if there were any laboring mamas who might need my doula services. The charge nurse introduced me to your nurse. I liked his energy and fashion style. Red tennis shoes is not something I see often with scrubs.
You were 5 centimeters dilated and were laboring like a pro when I quietly entered your dimly lit room. You sat on a birth ball, eyes closed breathing through a contraction. Your husband sat next to you and applied pressure on the spot in between your thumb and pointer finger. You had a calm about you that made sense for having done this a few times before.
When the contraction ended, your nurse introduced me and I offered my doula services. I noticed your water cups were nearly empty so I left your room and filled them up. When I returned I asked permission rub your shoulders. Who says no to this? Not you. You closed your eyes and breathed through a contraction. I took a deep breath with you. Our partnership had begun.
I invited your exhausted husband to take a nap. We transformed the hospital couch into a bed. His snores filled the room. You continued to contract while I rubbed you shoulders reminding you to breathe.
Girl, you were so calm and brave. The contractions built with intensity and as did your internal focus. In between contractions, we talked about your other five births. I heard about your first long labor; your second short labor. Your third birth was particularity exciting. After driving to Salt Lake City from Evanston, Wyoming and checked into the hospital. Your two small kids were with you then more family showed up creating chaos. The hospital room was not big enough so you asked the nurse if you could leave and labor at home. Surprisingly, she agreed. You left the hospital and headed home. You labored at home a little too long and your son was born in front of the church on West Temple. You laughed retelling the story.
Your forth and fifth births were less eventful. You contracted for awhile, and then labor stalled at a six centimeters. A few hours later, the contractions picked up. You fully dilated pushed the babies out quickly. Your fifth baby arrived fast. So fast that your husband missed it because he was out getting food and didn’t return in time.
This labor started around midnight. By 2am your contractions kept you awake. Your water broke at 3am and and you arrived at the hospital at 4:30am.
By the time I met you at 8:30am, you’d been in labor for over eight hours. It was 2pm when exhausting set in. You had been dilated at 6cm for a few hour and you asked for an epidural. After receiving it, you were immediately happier, more relaxed and ready for a nap.
We turned out the lights and you slept. I sat and read next to you as you peacefully slept and your husband brought lunch to the kids at home. Occasionally the nurse came in to move you around. because your baby was having a “temper tantrum” meaning that her heart was dipping during your contractions. You laid on one side and fell asleep and then we’d move you to your other side. Around 4pm your husband walked in. Happy to see you sleeping, he walked back to the couch and took his second nap of the day.
At 5pm you changed positions again. When he moved you from your back to your left side your contractions picked up. Even with the epidural, you felt intense sensations. You asked your nurse to increase your epidural. Since the baby was moving down into the birth canal the epidural didn’t touch the pain. You focused once again knowing this birth was near.
Your husband woke up and went to the bedside. He held your hand while I pressed down on your hip to give you counter pressure. You wrapped your free hand around the bed rail and closed your eyes.
A few contractions later you said, “I have to push. I feel like I have to push. Her head is right there.”
I walked out to find you your nurse and he came in and checked your cervix. You were complete at 10cm. “Let’s have a baby!” he said joyfully.
A half hour later the baby team was assembled. Your focus was not birthing the baby before the doctor arrived which was hard. Your body was ready to have this baby.
A few minutes later, an OBGYN walked in the room. While he slipped into scrubs, you sat up and opened your legs. Seconds later your daughter was born. It was the fastest birth possible. Her healthy cry filled the room. One of the nurses pronounced it was a girl at 6:02pm. She was placed on your chest and your husband cut her umbilical cord. It was a gorgeous scene.
While you held your baby skin to skin, the staff attended the delivery of your placenta. They cleaned you up and your husband took photos of the baby with both his phone and the Polaroid camera. I held you baby girl when she was forty minutes old. Her lips puckered making a guppy face. I knew she was ready to nurse. I handed her back to you. She found your nipple and latched on.
I said good bye to you and your family right before 7pm. You were so kind with your appreciation and gave me of the Polaroid photos. I really appreciated being a part of your labor and birth of your daughter. She is a miracle.
An OMazing Movement: Doula Support for all!
I am starting an OMazing movement. Doulas for all; during and after the birth. We need everyone’s help. I support mamas in my community with their birth journey, which is fantastic on the micro level. Through education, yoga and support in the birth room, I am making a difference. However, I am limited to the number of women I support. We need to work on the macro level.
I want to create a wider net of doulas, friends, and compassionate supporters. My mission is for every woman who wants that support will have access to a compassionate, kind and calm support person at and after their birth. Partners are wrapped up into their own journey. Women really need a third party support person. This doula work will be karmic. Women will take a turn giving support and then either they personally will receive the support or someone they know and love will.
Certified professional doula services cannot be underestimated. Their services are magical. However, so many laboring mothers either are not familiar with or can afford a hired doula. How can we change that model and create this movement? Midwives, doctor and medical assistants offer medical advice and perform procedures but mamas need more. Did you know that nurses spend on an average 6% of their time with patients?
My book club met this week and we shared birth stories. I was reminded of doula impact during and after birth and energized me once again to focus on spreading the message. Five of us reflected on how hard our birth and postpartum experience was at the time, especially when we were alone.
· One of my friends remembered complications after her cesarean section. This was her third cesarean and her husband and two infant boys were home sick. Left in the hospital alone with her new born baby she struggled. She was in tremendous pain, lonely and miserable.
· My second friend’s water unexpectantly broke at 37 weeks. She was grateful that she had a hired a doula who took immediate charge. She recommended a couple non-medical techniques to start labor. They walked. stimulated her nipples and the doula did acupressure on her feet. The stimulation and movement successfully started her labor and her son arrived the next day.. After the was in the NICU for a few days he was released. My friend’s fear showed up at home. Paranoid that he’d stop breathing, she set up camp next to his crib. Alone, next to her baby, her emotions ran wild.
· My third book club friends delivered a baby girl a few months after my second friend. Her husband said that he’d be the doula so that was that. I asked how that went and she laughed. Although her husband was helpful in labor, she admitted going home was rough. Totally overwhelmed it didn’t take long for her to break. She called her friend who quickly came over, marched in, and took control. She showed her how to swaddle the baby, supported her nursing and just listened. She was the post natal doula support that she desperately needed.
· The final birth story was told by a friend hired a doula for both the birth and postpartum. After the bonding experience of the birth, she was so happy to have the same doula in her home offering for the first six weeks of the baby’s life. It was a game changer. The doula showed my friend how to care and feed the baby. She cooked and cleaned. My friend said she couldn’t imagine her experience without a doula. She recommends it to any and everyone.
If you don’t have a doula, you need a friend - and one who will show up. Show up at your birth. Show up at your house afterwards. If they need some tips on what to do, have them email me: omazingbirth@gmail.com. I can guide them.
The OMazing Birth
Welcome to OMazing Blog. I kick it off with a birth story. Not the birth of a baby, but the birth of my new business.
A handful of years ago, my friend Carly asked me to marry her and her fiancé Jaime. Honored by the request, I said yes. A few months after her wedding, she was pregnant. Carly told me one summer afternoon, after practicing yoga in the park that she couldn’t find a doula. She casually said, “I wish you were a doula. You’d be a great doula. Will you be my doula?”
Surprising myself, I responded , “sure!” I had no idea what being a doula entailed, but I’d do anything for Carly and I knew I’d figure it out. I attended a local weekend workshop with Salt Lake City’s doula training guru, Kristi Ridd-Young who taught me the basics. I took my new knowledge to Carly’s labor on a Sunday afternoon in November, 2016. The power and determination of Carly’s unmedicated birth inspired me to continue on the doula path. I realized that I wanted to be a surrounded by the miracle of birth and my doula support made a difference in her daughter Layla’s birth.
What did I do that afternoon that made such an impact? I showed up and served. Doula means “servant” in Greek. The essence of a doula’s work is simply being with a laboring mama and telling her that she is powerful and safe. I reminded Carly to breathe. I offered her sips of water in between contractions. I showed her husband ways to comfort her. I stayed close to Carly throughout her labor, birth and postpartum.
After that experience, I continued my training with Birth Learning and completed a twelve week Advance Doula course. I registered to certify with DONA(Doulas of North America). Six months later, I travelled to Tacoma, Washington and spent a weekend with Kelli Barr-Lylesat a childbirth education workshop. I wanted to learn as much as I could about the birthing process.
All this time, I worked at a non-profit supporting Park City’s public schools. I assisted with a few births here and there and dreamt of starting a baby business. In August, 2018 I left my job and the United States. My ten year old daughter, fourteen year old son and I moved to France for the semester. The three of us lived in a small apartment in Provence. The kids attended a French school. I practiced French yoga, shopped at local markets, planned weekend travel and blogged. My amazing husband stayed in Park City and funded our fun.
Sadie’s first day of school in France
I resisted the temptation to plan my new business at a French café. Instead, I wandered around Aix-en-Provence and practiced curiosity. The adventure was extraordinary and I returned to Park City rejuvenated and ready to start OMazing Birth.
I spent the next few months connecting with health professionals and learning the local birth landscape. I realized there some fantastic birth services in Park City however there is not a clear hub for the pregnant and prenatal community. Prenatal yoga classes are sporadic and most of the doula and childbirth classes are offered in Salt Lake City. There is an active Facebook group however, I believe there still is a need for community. New mamas need each other!
Being a passionate yogi, I wanted to incorporate prenatal yoga into my new business. In March, I attended a ten day prenatal yoga certification training in San Francisco. I returned home and started teaching classes at my house. My plan is to turn our studio apartment into a yoga studio this summer. In the mean time, I created the OMazing website and started volunteering as a doula at the University of Utah Hospital.
The volunteer work reminds me of the importance of doula support. We need more doulas in this world! I hate to think of woman laboring alone or experiencing negativity in their birth room. The medicalization of birth seems to be at an all time high. (More on that later) Therefore the need of doulas is at an all time high. Spread the word!
Last week, I supported a beautiful Cameroon woman in labor named Rose Marie. She was alone until I arrived to my volunteer shift. Together we breathed and focused on her labor. I held her hand and reminded her to trust her body.
Rose Marie admitted that she was nervous to be alone in childbirth. A few days prior, her African friend told her to pray and that her angels would send her someone, even if it was someone she did not know. She showed me the text exchange. How wild it must have been when I showed up in her room? She told me later that she knew God sent me.
I stayed with Rose Marie though the night. At 3am, after almost 36 hours in labor, the doctors rolled Rose Marie into the operating room for a cesarean section. Dressed in scrubs, I stood at her head and rubbed the spot on her forehead in between her eyes. I photographed her baby girl as she came out of her stomach before being whisked away to the NICU. Rose Marie stared at the photo while patiently to meet her baby. Her baby, Annadisa has a heart condition and is still in the NICU. She needs all of our prayers!
I arrived home at 6:30am the next morning just in time to wish my son a good day at school. I went straight to bed. As my head hit the pillow, I marveled at Divine Intervention. Was Rose Marie’s prayer that powerful? Did the angels send me to her? I believe they did but of course I don’t know. However, I know that OMazing Birth is here for a reason. I am in the right place at the right time.
Welcome! Thank you for joining me on this journey.
Sara